ABB Smile Makeover

Treatment carried out by Salman Siddiqi

Dr Salman Siddiqi is an associate dental surgeon at Thornaby Dental Centre and Grace Dental Care, Stockton on Tees. He became a certified provider of the IAS Inman Aligner in June 2015 and enjoys providing minimally invasive aesthetic dental treatments with particular focus on AAO combined with bleaching on bonding. He also enjoys providing treatment for highly anxious patients on the local sedation service and motivating them to a better oral health status.
Anterior alignment orthodontics (AAO) has created a paradigm shift in modern cosmetic dentistry and influenced current thinking in our approach to anterior aesthetic cases (Qureshi, 2010). Recent studies have shown adult orthodontic treatment not only provides improvements in dental aesthetics but also has a significant positive impact in the psychosocial aspects of the patient’s life (Gazit-Rappaport, 2008).
The minimally invasive philosophy which extends across the IAS Academy teaching syllabus ensures GDPs like myself provide safe, predictable outcomes for patients and avoid an early transition into the ‘restorative cycle’. I have been a keen user of the Inman Aligner since completing the hands-on course in 2015 and find it to be an invaluable tool in treating patients who present with concerns about their anterior dentition.
The Inman Aligner is a highly effective and unique evolution of the traditional spring retainer and uses super-elastic Nickel-Titanium open coil springs to move upper and lower anterior teeth. Very light but consistent forces are provided by the spring mechanism, enabling correction of anterior crowding, rotations and some types of spacing (Qureshi, 2008).
The following case was treated recently using the Inman Aligner combined with some external bleaching and composite bonding.
Patient background
A new patient presented to our practice requesting some improvement to her existing smile. Her main concerns discussed at the consultation appointment were her ‘flared’ and ‘prominent’ upper front teeth. She was becoming conscious of the fact that her overjet was gradually increasing and making the spacing between her upper front teeth more prominent. She reported having removable orthodontic treatment with a twin block appliance as a child, but didn’t recall any retainer being given at the end of treatment.
The patient’s main treatment goals were to reduce the overjet, close the spacing/diastemas and improve the overall colour of her smile.
Orthodontic Assessment
A thorough assessment was initially carried out including an orthodontic assessment, full IAS Academy protocol photos (figure 1) and digital calliper measurements of upper 3-3. The IAS assessment forms allow for a very comprehensive record to be completed efficiently and are invaluable when reviewing the salient features of the patient’s malocclusion.
| Measurement | Result |
|---|---|
| Skeletal | Moderate Class II |
| FMPA | Average |
| Lower Face Height | Normal |
| Facial Asymmetry | None |
| Soft Tissues | Lips competent at rest | Average Lip line |
| Overjet | 8-9mm |
| Overbite | Increased with 40% coverage lower incisors |
| Crossbite | None |
| Displacement on Closure | None |
| Incisor Relationship | Class II division I |
| Molar Relationship | Class III ½ unit | Class III ¼ unit |
| Canine Relationship | Full unit Class II | ¾ unit Class II |
| Teeth Present | 764321 | 123467 | 7654321 | 1234567 |
| Centrelines | Lower deviated to left by 3-4mm |
Orthodontic Diagnosis
- Moderate skeletal class II base
- Average FMPA
- Lips competent at rest
- Class II div 1 Incisor relationship
- RHS full unit class II molar relationship
- LHS ¾ unit class II molar relationship
- RHS ¾ unit class II canine relationship
- LHS ¾ unit class II canine relationship
- Overbite increased (40% coverage lower incisors)
- Overjet increased at 9mm
- Dental centre non-coincident with lower 3-4mm to the left of the facial midline
- 2mm crowding and 8mm spacing upper arch
- 3mm crowding lower arch
Treatment options
A full discussion was then carried out with the patient explaining the options available to meet her treatment goals.
Given the marked class II division I malocclusion, a specialist orthodontist referral was offered to consider fixed appliance treatment in conjunction with orthognathic surgery. We also discussed the possibility of using indirect/direct restorations only to meet her treatment aims, but highlighted the risk of further orthodontic relapse which would inevitably increase the overjet. A discussion was also had about the high biological cost of potentially heavy preparations, which would be needed to reduce the overjet. The patient was not keen to wear a fixed appliance and wanted to focus on a more flexible solution given her busy working lifestyle.
The Inman Aligner was discussed, including the benefits and limitations of the appliance. I explained that a course of AAO would have low impact on the structural integrity of the unrestored anterior teeth, unlike indirect restorations. The compromises of the appliance were also deliberated, in particular that posterior teeth would not be moved, some small diastemas would still remain at the end of treatment and the skeletal class II discrepancy would not be corrected.
Treatment planning
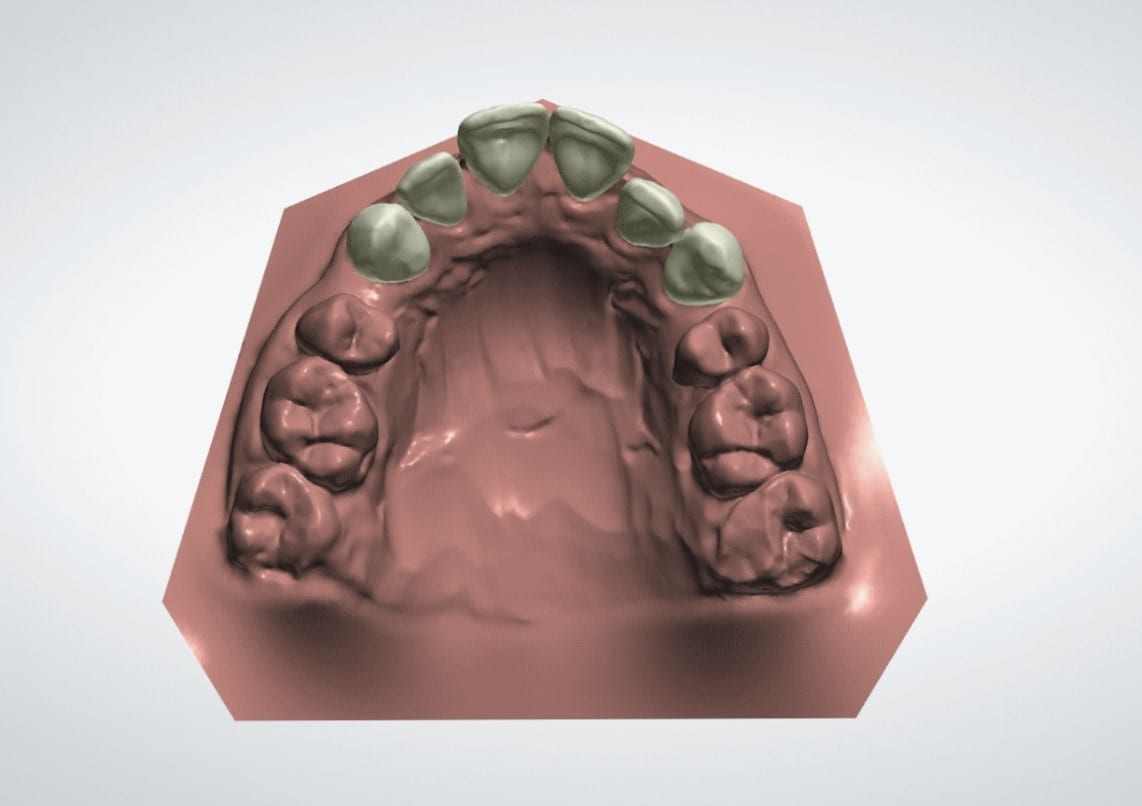
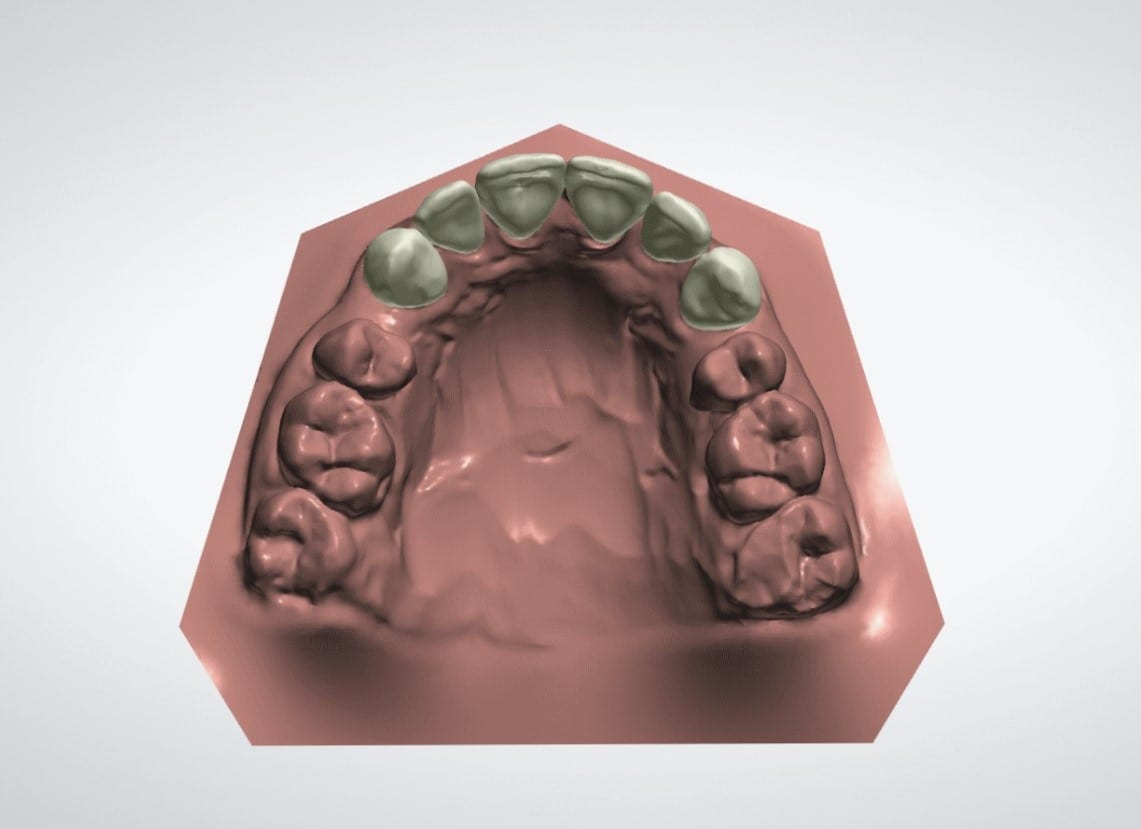
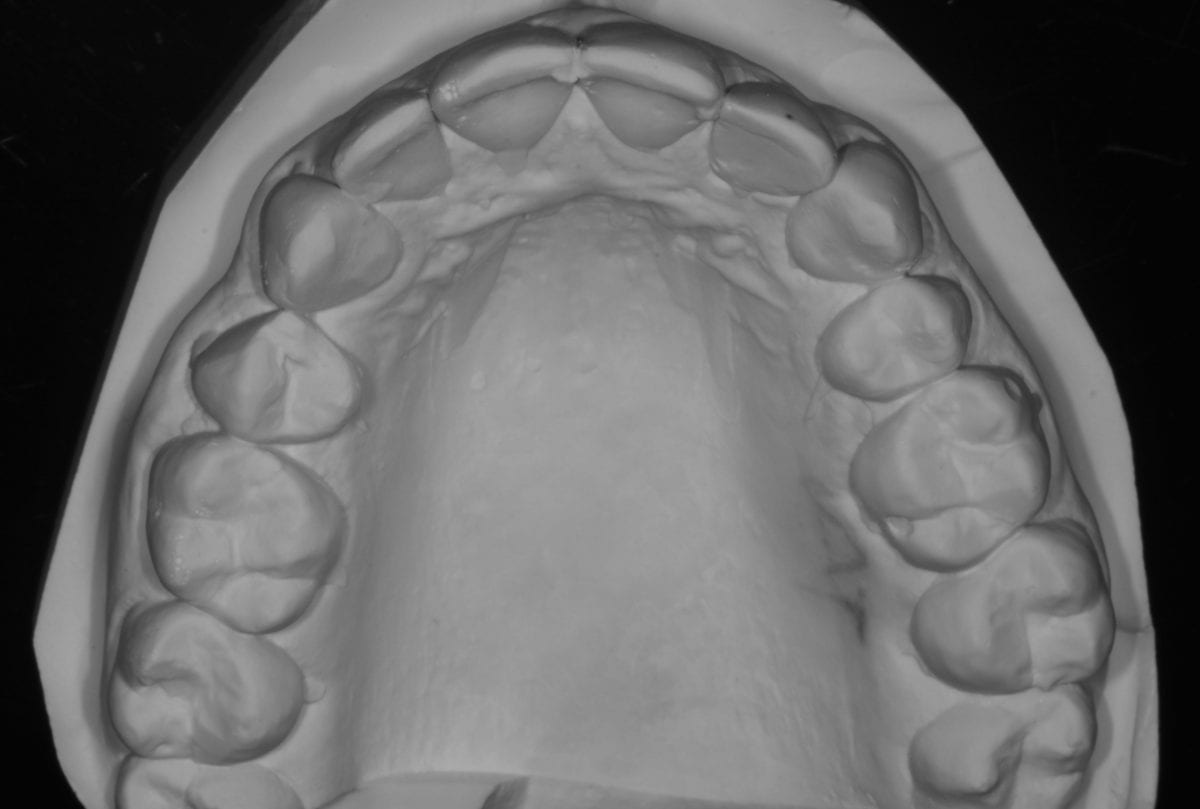
A quick chairside Spacewize+™ digital analysis (figure 2) showed simple anterior alignment and reduction of the overjet could be achieved within limits. I explained some spacing would remain following completion of the alignment and offered composite bonding the close any residual diastemata or spaces. The patient liked the minimally invasive solution that the Inman Aligner would allow and was keen to proceed with treatment. An Archwize™ digital plan (figure 3) and a corresponding 3D printed model made by the IAS lab were then used to allow fully informed consent for treatment. The 3D printed model (figure 4) allows an excellent simulation of the final proposed setup and was key in allowing the patient to fully visualise the plan before treatment commenced.
Problem list:
- Mod Skeletal Class II
- Class II division 1 incisors
- R full unit class II molar, L ¾ unit class II molar
- R and L ¾ unit class II canine
- Upper and lower mild anterior crowding
- Upper labial spacing
- Diastemata present between and distal of centrals and distal to canines (more prominent UR34)
- Chipped incisal edge UL2
Ideal treatment aims:
- Correct Class II skeletal
- Correct class II div 1 incisor relationship to class I
- Correct molars and canines to class I
- Relieve all upper and lower crowding
- Close all spacing upper labial segment
- Composite restoration UL2 incisal edge
Compromised/AAO treatment aims:
- Accept Class II skeletal base
- Reduce overjet in class II division 1 incisor relationship
- Accept molars and canines
- Relieve upper crowding, accept lower crowding (provide retention)
- Close residual spacing with composite bonding after alignment
- Composite restoration UL2 incisal edge
Treatment provision
Alignment
PVS impressions of both arches, a bite registration and clinical photos were sent along with a prescription to the IAS lab. An Archwize™ 3D plan was then returned six days after sending the impressions, which I approved following review. The Archwize™ shows the proposed final position of the teeth after anterior alignment and gives a visual ‘mock up’ of the before and after.
The Inman Aligner was sent back to me the following week and fitted for the patient. The total IPR figure was very low at just 0.90mm as spacing was already present. I performed half of the total IPR at the first appointment and placed a composite anchor on UL2, which was the most ‘in-standing’ and palatally crowded tooth.
The patient was reviewed at two-weekly intervals for further IPR and replacement of composite anchors as needed. Occlusal and retracted photographic views were recorded at each review appointment, acting as a valuable tool in achieving good patient compliance and progressing the case more efficiently (figure 5). A significant reduction in the overjet and closure of spacing was achieved over 12 weeks by retracting the central incisors and providing mild tipping of UL2.
Bleaching
External tooth whitening was performed over two weeks using 10% carbamide peroxide. Retention was maintained using the Inman Aligner during the whitening phase of treatment.
Bonding
To finish off, composite bonding (figure 6) was carried out under full rubber dam isolation to the following areas:
- Build up the worn UL2
- Direct composite veneer UR2
- Edge bonding to reshape the embrasure space between the centrals
- Diastema closure between UR3-UR4
A growing body of current evidence supports that relapse towards the patient’s original malocclusion can occur post treatment as a result of periodontal, gingival, occlusal and growth related factors (Littlewood et al, 2017). To reduce this risk, long-term retention was provided for this patient using a bonded inter-canine wire retainer and an Essix appliance.
Outcome and case appraisal
The patient was pleasantly surprised with the outcome (figures 7 ) of her treatment and impressed at how close to the 3D Archwize™ model the finished result was (figure 8)! I was able to deliver a minimally invasive treatment outcome to meet the patient’s initial aims and finish the case within her requested timeframe.
The IAS online mentor support I have received since completing the Inman Aligner course three years ago has been second to none and pivotal in allowing me to treat a wider variety of anterior alignment cases. The potential of the appliance combined with bleaching and bonding techniques has transformed my own clinical practice for patients seeking cosmetic smile improvements.
I would like to thank the IAS Academy mentors and lab team for their continued help and support as without them I can’t deliver the high-quality cases I aspire to achieve every time. I’d also like to thank Dr Tif Qureshi for his continued feedback and mentoring in helping me improve my knowledge of the Inman Aligner and giving me the confidence to tackle more challenging cases. His recent ABB course allowed me to put the crucial finishing touches to my anterior alignment cases and has truly been a game changer! Thanks also to all the team at Thornaby Dental who work so hard and support me daily.
 Row 1 Assessment
Row 1 Assessment  Row 2 Assessment
Row 2 Assessment  7a Row 1
7a Row 1  7b Row 2
7b Row 2