To Prove a Negative
That is the question? How, do you prove something is not what it is?
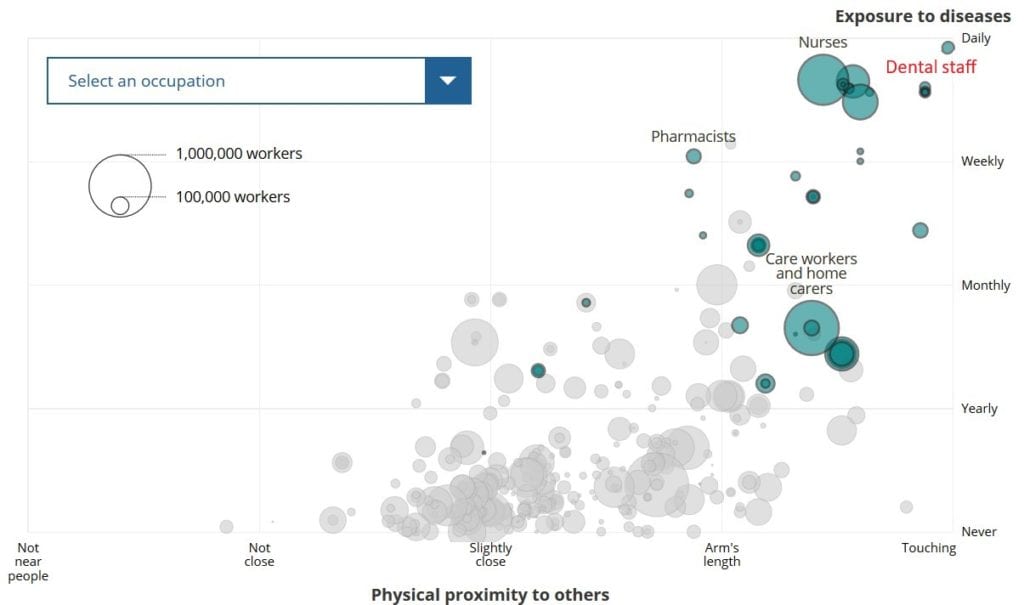
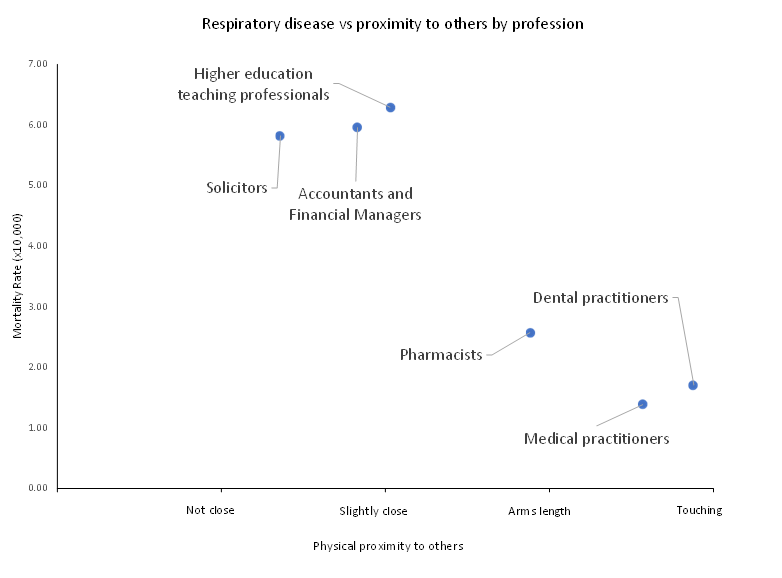
In dentistry this is now an extremely important question as we are being told the ‘Dental practices are COVID heaven’ (Prof Mike Lewis; TV interview); Dentistry creates aerosols and hence these aerosols are dangerous and transmit COVID. The fact that that these are now defined as AGPs (Aerosol Generating Procedures) and by having its own acronym implies it is an important and significant issue.
We are being influenced by the opinion of personalities and supply companies to apply a significant of number costly and time inefficient solutions ie no AGPs, ‘sterilisation’ of surgeries, room extraction to name a few. But where is the evidence to support these, when challenged we are directed to research that shows:-
That the upper respiratory tract is where COVID virus is shed and that (medical) AGPs ie tracheal intubation, non-invasive ventilation, tracheostomy, CPR, manual ventilation before intubation and bronchoscopy. These are the WHO listed AGPs, note that dental procedures are not included, which is at odds with the UK interpretation of what defines an AGP.
That COVID virus can be found in breath, coughs and sneezes and that the virus can survive for about 2 hours. That COVID can survive on certain hard surfaces for up to 72 hours.
This research is undertaken in LABORATORY conditions where the conditions are set up to maximise the opportunity for the virus being detected and surviving, not real-life indoor or outdoor situations.
So, on the face of it, the evidence is overwhelming, that dentistry creates aerosols and hence is dangerous to both staff and patients!
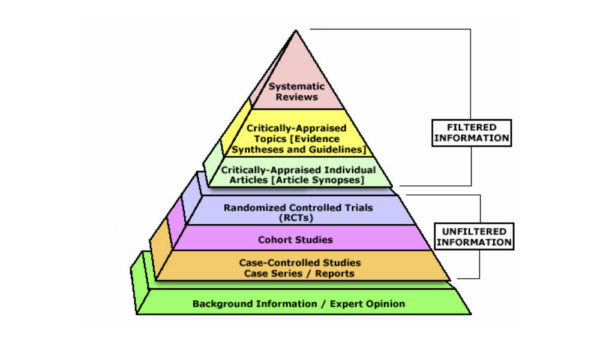
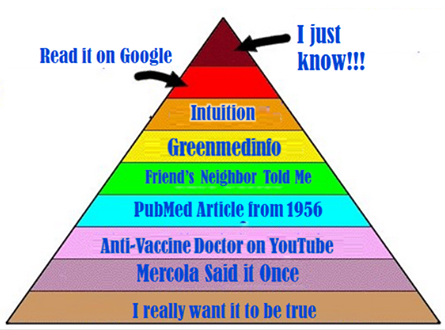
So how do we challenge this righteous stance? We have to prove a negative. However, as those of us who have tried to enter into a scientific debate of opinion with marketing companies and personalities we rapidly enter the world of pseudoscience and facts get left behind. The images below are to remind us of the evidence pyramid and its pseudoscience counter.